In the early 1970’s at the University of Rochester, a multidisciplinary research team uncovered some puzzling new data. The immunologist, Nicholas Cohen, and the psychologist, Robert Ader, were collaborating on a research project studying taste aversion in rats. They were giving rats a saccharin solution to drink, followed by an injection of Cytoxan, an immunosuppressive drug that has an unpleasant side effect of gastric distress. As expected, upon repeated exposure to the saccharin and the drug, the rats learned to avoid drinking the sweet solution, which is an acquired behavior called conditioning. However, among the behaviorally conditioned rats the researchers noticed another and more surprising phenomena: when they gave the conditioned rats large amounts of saccharin solution, many of those rats later died. Moreover, it seemed that both the behavioral avoidance and mortality rate correlated to the volume of saccharin solution the conditioned rats had been administered.
Fast forward a few years, and Ader and Cohen were able to test, confirm and publish the fascinating reason why these rats were dying after taking only saccharin. They discovered that the experimental procedure allowed the rats to develop two types of conditioning. The first was the expected pairing of the saccharin taste and the gastric discomfort, which lead to the behavioral outcome of making the rats drink less saccharin. The second and more surprising type of conditioning was the pairing of the saccharin taste and the suppression of the immune system, which meant that for conditioned rats consuming large amounts of saccharin had the same effect as an overdose of an immunosuppressant drug. More specifically, the conditioning allowed the neuronal circuits that detected the saccharin taste, to impact the function of the immune system
The mind-body question is a longstanding philosophical debate over whether and how thought, emotions and consciousness, which are associated with the abstract concept of ‘mind’, interact or relate to the physical body and the brain. In the 17th century, a version of this question was addressed by René Descartes, who discussed whether the mind is distinct from the physical body. Descartes argued that mind and matter are inherently different: One consists of physical matter and the other not, and therefore one cannot interact with the other. However, over the centuries, biologists adopted a different version of this question. In fact, the field of neurobiology is built around the assumption that all mind-related abilities such as cognition, emotion and even awareness carry a chemical and physiological basis
One of the most important and well-known aspects of the neuro-immunological investigation focuses on the endocrine system and its role as a pathway mediating the effects of mental stress on physiology. The endocrine system regulates a range of physiological functions via the release of hormones, and is one of the major pathways that allow the central nervous system to regulate physiology in general, and in particular peripheral immunity. In the 1930s, Hans Selye developed the idea that stress is able to promote symptoms of illness
New technological developments allowed researchers to descend deeper into the molecular level, and explore how life circumstances and emotional reactions shape the gene expression profile of immune cells
Besides the HPA axis and other endocrine pathways, there are several neuronal networks that connect the brain with the body. Two of those networks were shown to be able to modulate immunity. Upon activation, both the autonomic and sensory neurons release several neurotransmitters and neuropeptides, which can impact immune activity. Research discovered that immune cells express the receptors for these factors
For many decades the nervous system and immune system were studied independently. With that said, it is now recognized that these systems communicate, and that these complex connections greatly impact physiological adaptation both in health and disease. Continued research in this area will, hopefully, be able to provide new therapeutic advances.
1. Ader, R. & Cohen, N. Behaviorally conditioned immunosuppression. Psychosomatic Medicine 37, (1975).
2. 2Giang, D. W. et al. Conditioning of cyclophosphamide-induced leukopenia in humans. The Journal of neuropsychiatry and clinical neurosciences 8, (1996).
3. 3 Longo, D. L. et al. Conditioned immune response to interferon-gamma in humans. Clinical immunology (Orlando, Fla.) 90, (1999).
4. Vits, S. et al. Behavioural conditioning as the mediator of placebo responses in the immune system. Philosophical transactions of the Royal Society of London. Series B, Biological sciences 366, (2011).
5. Ader, R. & Cohen, N. Behaviorally conditioned immunosuppression and murine systemic lupus erythematosus. Science (New York, N.Y.) 215, (1982).
6. Lysle, D. T., Luecken, L. J. & Maslonek, K. A. Suppression of the development of adjuvant arthritis by a conditioned aversive stimulus. Brain, behavior, and immunity 6, (1992).
7. Barrett, L. F. The Future of Psychology: Connecting Mind to Brain. Perspectives on psychological science : a journal of the Association for Psychological Science 4, (2009).
8. Schiller, M., Ben-Shaanan, T. L. & Rolls, A. Neuronal regulation of immunity: why, how and where? Nature reviews. Immunology 21, (2021).
9. Selye, H. Thymus and Adrenals in the Response of the Organism to Injuries and Intoxications. Br J Exp Pathol. 17, 234–248 (1936).
10. Szabo, S., Tache, Y. & Somogyi, A. The legacy of Hans Selye and the origins of stress research: a retrospective 75 years after his landmark brief “letter” to the editor# of nature. Stress (Amsterdam, Netherlands) 15, (2012).
11. Tan, S. Y. & Yip, A. Hans Selye (1907-1982): Founder of the stress theory. Singapore medical journal 59, (2018).
12. Nicolaides, N. C., Kyratzi, E., Lamprokostopoulou, A., Chrousos, G. P. & Charmandari, E. Stress, the stress system and the role of glucocorticoids. Neuroimmunomodulation 22, (2015).
13. Cruz-Topete, D. & Cidlowski, J. A. One hormone, two actions: anti- and pro-inflammatory effects of glucocorticoids. Neuroimmunomodulation 22, (2015).
14. Cole, S. W. Human social genomics. PLoS genetics 10, (2014).
15. Cole, S. W. et al. Social regulation of gene expression in human leukocytes. Genome biology 8, (2007).
16. Miller, G. E. et al. Greater inflammatory activity and blunted glucocorticoid signaling in monocytes of chronically stressed caregivers. Brain, behavior, and immunity 41, (2014).
17. O’Donovan, A. et al. Transcriptional control of monocyte gene expression in post-traumatic stress disorder. Disease markers 30, (2011).
18. Antoni, M. H. et al. Cognitive-behavioral stress management reverses anxiety-related leukocyte transcriptional dynamics. Biological psychiatry 71, (2012).
19. Black, D. S. et al. Yogic meditation reverses NF-κB and IRF-related transcriptome dynamics in leukocytes of family dementia caregivers in a randomized controlled trial. Psychoneuroendocrinology 38, (2013).
20. Pert, C. B., Ruff, M. R., Weber, R. J. & Herkenham, M. Neuropeptides and their receptors: a psychosomatic network. Journal of immunology (Baltimore, Md. : 1950) 135, (1985).
21. Blalock, J. E., Harbour-McMenamin, D. & Smith, E. M. Peptide hormones shared by the neuroendocrine and immunologic systems. Journal of immunology (Baltimore, Md. : 1950) 135, (1985).
22. Kohm, A. P. & Sanders, V. M. Norepinephrine and beta 2-adrenergic receptor stimulation regulate CD4+ T and B lymphocyte function in vitro and in vivo. Pharmacological reviews 53, (2001).
23. Xie, Y., Frede, S., Harnish, M. J., Exton, M. S. & Schedlowski, M. Beta-adrenoceptor-induced inhibition of rat splenocyte proliferation: cytokine gene transcription as the target of action. Immunobiology 206, (2002).
24. Szelényi, J., Kiss, J. P. & Vizi, E. S. Differential involvement of sympathetic nervous system and immune system in the modulation of TNF-alpha production by alpha2- and beta-adrenoceptors in mice. Journal of neuroimmunology 103, (2000).
25. Tracey, K. J. The inflammatory reflex. Nature 420,.
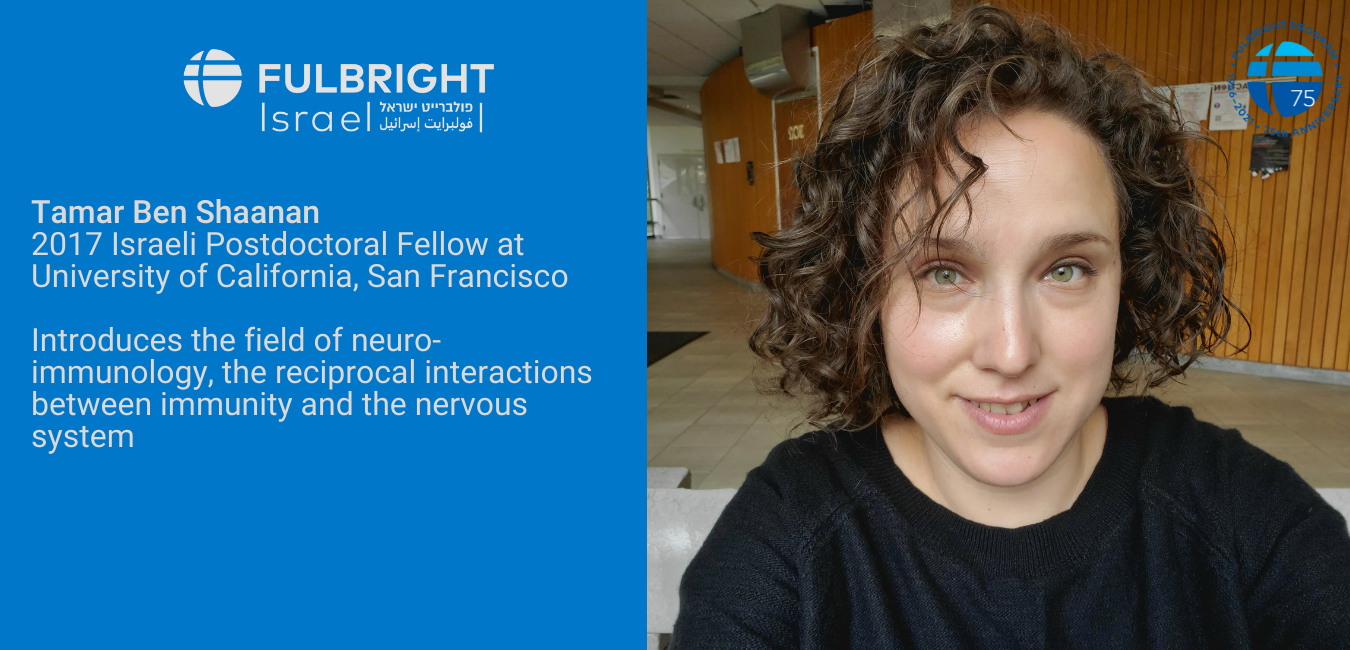
Articles are written by Fulbright grantees and do not reflect the opinions of the Fulbright Commission, the grantees’ host institutions, or the U.S. Department of State.


